Rita H. Khoury, MD; B. P. Salmon, MS; Asha Gandhi, BS; Prital Patel, BS; Peter Gudaitis, BA; Dauna Gudaitis, BA
(2013) Abstracts and Case Studies From the College of American Pathologists 2013 Annual Meeting (CAP ‘13). Archives of Pathology & Laboratory Medicine: October 2013, Vol. 137, No. 10, pp. 1343-1526.
Context: Carbapenem-resistant Enterobacteriaceae (CRE) are a family of bacteria that are resistant to several classes of antibiotics including one of the carbapenems. Klebsiella species and Escherichia coli and Enterobacter species are the most common enterobacteriacae reported. These bacteria produce enzymes that break down carbapenems and make them ineffective. Invasive infection with CRE has been associated with mortality rate greater than 40%, which makes CRE a big threat in every health care setting, especially in long-term care facilities (LTCFs) because of the age-associated risk factors.
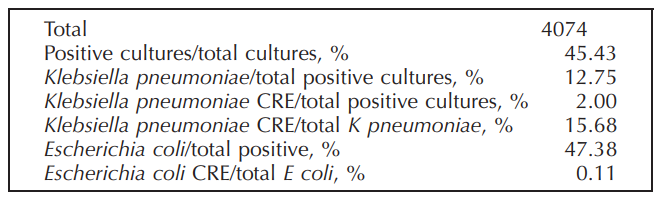
Design: We collected 4074 urine specimens for culture from residents in long-term care facilities during a period of 4 weeks. All positive cultures were subcultured and then identified by using MicroScan Walkaway 96 conventional panels; the isolate was considered CRE if it was resistant to 1 or more of the carbapenems.
Results: Of the total patients, 1851 had a positive culture and 38 had a CRE-positive culture; 37 cases were due to Klebsiella pneumoniae (either extended-spectrum β-lactamase or multidrug resistant), and 1 was due to multidrug resistant E coli.
Conclusions: Long-term care facilities are high risk for CRE infection. Physicians should be aware and follow the CDC recommendations to implement the “detect and protect” strategies; infection control priority should be to identify the risk factors for CRE. The cautious and appropriate use of antimicrobial therapy for the treatment of suspected infections in residents of long-term care facilities is very important to prevent occurrence. In addition, it emphasizes the necessity for newer antimicrobial agents with activity against these organisms.

